It may seem like lupus and lung disease don’t have much in common. But around half of all people with systemic lupus erythematosus (SLE), the most common type of lupus, also deal with lung issues during the course of their disease.
Lupus causes inflammation in your body. This inflammation affects many parts of your body, including the joints, skin, and blood cells. Inflammation in your lungs can cause issues with:
- The membrane lining your lungs
- Blood vessels inside the lungs
- Your diaphragm muscle, which inflates and deflates your lungs
Though there are several lung conditions linked to lupus, many of them share symptoms such as pain and shortness of breath. If you have lupus and have lung symptoms, see your doctor
To know more about Lupus, Click Here.
Lung Conditions Tied to Lupus
Several conditions can show up as a complication of lupus. They include:
Pleuritis
This condition, also known as pleurisy, is the most common lung issue people with lupus have. Your lungs have a thin membrane that surrounds them called the pleura. The pleura also lines the inside of your chest cavity. It makes a small amount of fluid to keep the area it covers moving smoothly.
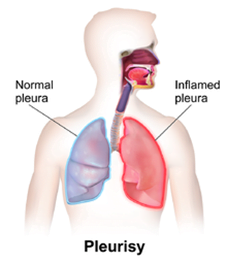
When the pleura gets inflamed because of lupus, it puts pressure on your lungs. Sometimes fluid builds up and can leak out (this is called a pleural effusion), which may cause shortness of breath or a cough.
Symptoms of pleuritis include:
- Severe, often sharp, stabbing pain in your chest
- Pain when you take a deep breath, sneeze, cough, or laugh
- Shortness of breath
Your doctor can diagnose it by looking at your chest on an X-ray along with other tests. To treat the pain and inflammation, your doctor may give you NSAIDs or steroid medications. Antimalarial medications such as hydroxychloroquine (Plaquenil) may also help prevent pleuritis.
Pneumonitis
When tissue in the lung itself is inflamed, your doctor may diagnose you with pneumonitis. Up to 10% of people with lupus get this condition. It can be serious and lead to permanent scars on your lungs.
You may get it because of a bacteria, virus, or fungus. Or your lungs may be damaged by an autoimmune injury when your immune system attacks your tissues as it would an infection. Pneumonitis may either be acute (severe and sudden) or chronic (slowly gets worse over the years). You don’t have to have had acute pneumonitis to get chronic pneumonitis, or vice versa.
Symptoms include:
- Fever
- Chest pain
- Shortness of breath
- Dry cough that may bring up blood
Chronic pneumonitis may come on slowly enough that you don’t know symptoms have started. Your doctor can treat it with a high dose of steroids or antibiotics. Some people need immunosuppressive medications. You may have scarring even if a treatment works. You reduce your risk of scarring and have better outcomes if you catch and treat pneumonitis early.
Pulmonary fibrosis
If inflammation in your lungs continues and does cause scarring, you can develop chronic diffuse interstitial lung disease or pulmonary fibrosis. The scar tissue on your lungs keeps oxygen from leaving your lungs to go into your bloodstream.
Symptoms include:
- Chronic dry cough
- Chest pain
- Trouble breathing during physical activity
- Tiredness and weakness
- Weight loss you can’t explain
Your doctor will want to rule out other causes such as infections. They can diagnose you with the disease by using a device called a spirometer to measure how well your lungs work. They may also use a peak flow monitor to see how fast you can blow air out of your lungs. Other tests include:
- Chest X-rays
- CT scan
Because the scars on your lungs are permanent, treatment can be difficult. Your doctor may recommend steroids to reduce inflammation, oxygen therapy, or pulmonary rehab. In some cases, you may need a lung transplant.
Pulmonary hypertension
Pulmonary hypertension is high blood pressure in the vessels that carry blood from the heart to the lungs. This condition strains the right side of your heart and prevents the right amount of oxygen from getting to your body. About 10% of people with lupus get it.
Symptoms include:
- Shortness of breath
- Swelling in your legs and feet
If it doesn’t get better, eventually you can have heart failure. To test for it, your doctor will do a blood test to test for a protein called brain natriuretic peptide (BNP). Your heart and blood vessels make more BNP when blood pressure goes up. They’ll also do some imaging tests:
- Chest X-ray
- Echocardiogram, which uses sound waves to make a moving picture of your heart as it beats
- Electrocardiogram, which measures your heart’s electrical patterns
If you have pulmonary hypertension, your doctor may be able to treat it with steroids and immunosuppressive medications.
Shrinking lung syndrome
About 1 in 6 people get this complication. When you have it, it seems like your lungs are getting smaller, making it harder for you to breathe well.
Symptoms include:
- Feeling out of breath
- Trouble expanding your chest all the way when you inhale
Your doctor may diagnose you using:
- X-ray
- High-resolution computed tomography (HRCT), which gives doctors a more detailed look at your chest cavity

Your doctor may prescribe steroids or immunosuppressive drugs to treat it. Pulmonary embolism (PE) A PE is a blood clot that blocks the arteries leading to your lungs. Typically they form somewhere else in your body and travel to your lungs. When you get one, you may feel:
- Chest pain
- Shortness of breath
- Anxious
- Faint or lightheaded
- A rapid or irregular heartbeat
You may also have trouble getting enough oxygen through your lungs. Your doctor can check to see if you have a PE using:
- X-rays
- CT scan
- Ventilation-perfusion scan (V/Q scan), a test that uses a small amount of a radioactive substance to examine the lungs
- Pulmonary angiogram, an X-ray image of your blood vessels
- Magnetic resonance imaging (MRI), which uses a magnetic field, radio waves, and a computer to show your doctor details of your organs and structures
- Duplex ultrasound is an ultrasound that shows the blood flow in your blood vessels
- Blood tests
- Electrocardiogram (EKG), which measures the electrical activity of your heart
You’re more likely to get this complication if you aren’t active, you have blood vessel damage, or you have antiphospholipid antibodies in your blood. To treat PE, your doctor might try one of these methods:
- Anticoagulants (blood thinners)
- Fibrinolytic therapy, or “clot busters,” medicines you get through an IV to break down life-threatening clots
- Vena cava filter, a small metal device doctors put in the large blood vessel that returns blood from the body to the heart
- Surgery
- Percutaneous thrombectomy, during which a doctor puts a long, thin, hollow tube (catheter) into your blood vessels to help break up a clot.
Who’s at Risk for Lupus-Related Lung Problems?
Certain populations have a greater chance of getting lupus-related lung conditions. These include:
- People with severe lupus. The more severe the lupus you have, the more likely you are to have lung problems.
- Women of childbearing years. Women who are between 15-44 have the highest risk of getting lupus in the first place, which puts them at risk of getting lung conditions.
- Minority groups. Black, Hispanic or Latino, Asian, and Indigenous people are more greatly affected by lupus than white people are. This puts women in these groups at the highest risk of all.
Try our product My Natural Lung Support for Healthier Lungs.